Whether intensive care places could be better coordinated, for example redistributed nationwide? “If you want, a lot is possible,” the doctor replies, but restricts: “However, this involves a lot of logistical effort: you don’t transport intensive care patients with a random ambulance.” In addition, transport naturally poses risks for patients.
This is another reason why Cornelia Dürkhäuser sits at home and waits to return to work in the hospital. She thinks the development in the health care sector in Germany is “very absurd”, says Dürkhäuser: “Until four weeks ago, I never expected that I would ever be threatened with short-time work. On the contrary, the workload has increased steadily since the beginning of my career.” However, she does not see the impending collapse of the health system, which is often discussed in the media because of the coronavirus. “At least not nationwide and not by Corona,” she adds. If anything, this collapse has been threatened for years by personnel policy and forced austerity.
„There is no need to register short-time work.“ – Statement of the Marburger Bund:

“We know from our membership surveys that doctors employed in the hospital work about 65 million hours of overtime each year. Compensation in leisure time in consultation with colleagues is certainly more sensible than applying for short-time work in the case of less work,” explains the Federal Association of the Marburg Confederation in a statement, adding: “Wherever the number of patients is currently lower, it is important to educate employees and train them for the treatment of COVID-19 patients.” In response to a small question from the fraction of Die Linke in the German parliament, the Federal Government also stated that short-time working was “not necessary to ensure the liquidity of the hospital.” For example, hospitals receive EUR 560 per unoccupied bed and day as a flat rate via the hospital rescue parachute, and the rescue fund also includes compensation for personnel costs. The German Hospital Society also points to this.
“You don’t turn it away with applause and one-off bonuses,” she says. Fundamentally better working conditions and sustainable pay are needed. In addition, the population had to move away from the claim “because of a gotten wood chip, at night at 3 in the emergency room. Unfortunately, such cases are now common there, which have actually nothing to do in an emergency room.”
However, more than short-time working Dürkhäuser deals with public misunderstandings about medical processes, especially the discussions about the coronavirus. “There are many things in the normal working life of an intensive care doctor that the normal population does not know, but which are now suddenly communicated publicly and are completely misinterpreted.” She names the triage as an example: this is used when the number of sick or injured patients exceeds the spatial and temporal treatment capacities: “This applies to a plane crash, a natural disaster and also to an infectious disease.” It is described as “the doctors simply let the patients die”. In the case of palliation and assisted dying, this is an elaborate intensive medical procedure.
In part, the medical doctor sees her profession as discredited and faces unjustified accusations. “This also complicates our day-to-day work,” emphasizes Dürkhäuser.
Decisions on coronavirus control not comprehensible
As a specialist, she wanted to stress that a disease like this should not be underestimated, but there is also no reason for “panicking”. Even though some of the protective masks had become scarce and were worn longer than usual, the hygiene measures were nevertheless relatively feasible throughout. “We have been able to deal with other epidemics in the past. Germany is very well positioned in the healthcare sector Our professionals are even admired abroad for their handling of the virus.”
“Toughly said” the politics only became aware of the work that medical personnel in Germany do on a daily basis through the pandemic. “Our profession, whether a doctor or a nurse, is suddenly in the spotlight,” Seif says. They would never have received as much recognition as they do today, even if they had long wished for it. “For so many years we have been fighting for more staff, more pay and more justified recognition,” she says. Unfortunately, bonus payments have only been announced so far, as it is unclear who will ultimately pay the money. “So now only Bavaria will certainly get a reward.”
Support for neighbours
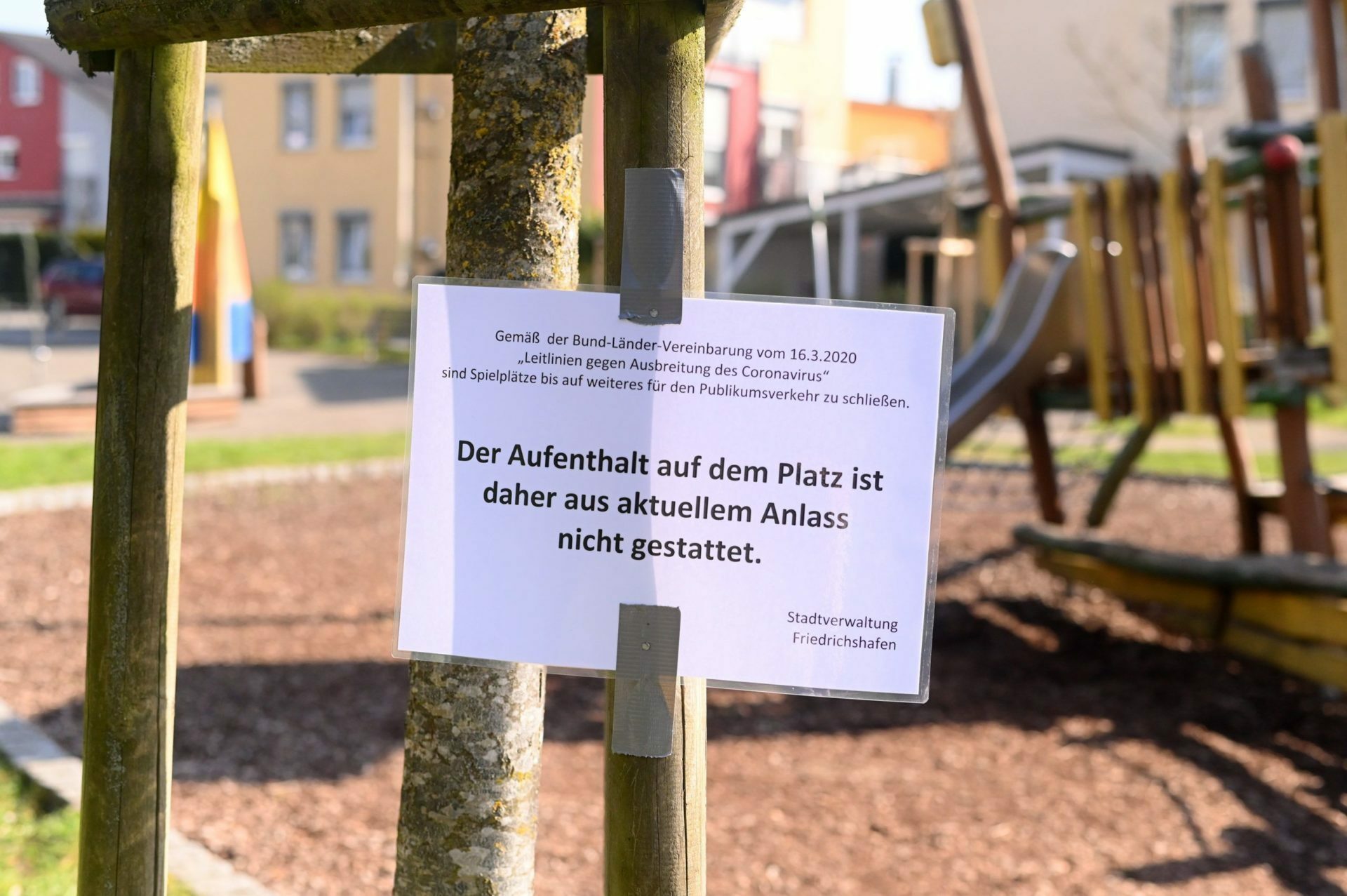
United in the shutdown, divided on easing
But when and how restaurants and tourism companies; Kindergartens, schools or cultural institutions will open, they handle differently – and for the affected sectors sometimes surprisingly short-term; sometimes the detailed restrictions for infection protective measures are revealed only one day in advance. Politicians say that this way, the can respond to the situation of the coronavirus regional and take the right steps.
Confusing rules
Court rulings
Largest aid package in history
More than black and white
Intensive care nurse Marie Krzykalla also observes misinterpretations of medical procedures through the presentation on (social) media and exchanges views with her colleagues: “The fact that medicine is portrayed in such black and white just bothers us a lot.” As an extreme example, she cites a headline in the Bild newspaper: “People die from the ventilator”. “Basically, that’s true, they die from the ventilator. But they die not because of the ventilator, but despite the ventilator,” Krzykalla comments. In the meantime, it has been shown that the majority of those who needed a ventilator in the course of a Covid-19 disease only needed it temporarily.
In fear of ventilators, Krzykalla sees a danger: “Perhaps people with symptoms who, the sooner they were treated, would require less invasive treatments, would come to the doctor or hospital much later for fear; this is a dangerous revolving door effect.”
In the video, she describes how the coronavirus is currently happening on her ward and how ventilation works:
That is why an understandable investigation into coronavirus is of great importance. Krzykalla cites the podcast by virologist Christian Drosten as a positive example, although his language is sometimes “very medical.” She wants a format that uses even simpler vocabulary. But she knows how difficult it is to explain: “You can’t teach people badly, there are no uniform symptoms, no uniform course, and no universal drug.”
Asked how she felt about the current debates about easing infection-protective measures, given her experience with Covid-19, she said: “I think it’s important that people are told much more precisely why the measure was introduced in the first place.”
Contact restrictions due to coronavirus additional load
Whether it’s eating together, taking a walk or just a smile: “They provide orientation through the daily visits,” says Härer. Physical closeness is particularly important: “A child can simply convey with the best love and closeness.” But the bans on visits would eliminate this and the nurses would have to compensate for this as much as possible. This makes it all the more important to pay more attention to the residents, combined with an increased effort and increasing documentation obligations. At the same time, protective masks and clothing made personal contact difficult, at least available, says Härer: “This makes it impossible to smile simply with the residents.”
In the same way, the situation is unusual for skilled workers and even more difficult to manage, since social contacts are largely dormant.
This only helps to a limited extent when people applaud from their balconies. She is very pleased with such recognition, confirms Härer. “But that doesn’t solve the tragic conditions that exist in our industry,” she says. This is the only reason why nurses are called heroes “because there are enough who work in sometimes dire conditions for the residents and out of professional honour”. She believes it is the luck of the industry that skilled workers in emergency situations are pushing even more to their limits.
At the moment, like Seif, she is particularly concerned that each state deals differently with the special burden on nurses caused by the coronavirus. Here promised bonuses, meals paid there and then support from the Medical Service of Health Insurance (MDK). “For me, it is not uniformly regulated and this has to be done nationwide,” says Härer. In order to improve conditions in the long term, she believes that the financing of the health sector should be changed: “This is the only way to raise the level.” On the one hand, this includes better pay and more recognition for work. At the same time, the benefits would have to remain affordable for those affected, and additional costs should not increase. Experts would have to look for solutions here.
Rapid development
Paramedic Andreas Durner also agrees with this attitude. “The trend over the last few weeks has been rapid,” he says. With new findings, processes have been regularly optimised and changed in his institution – this is to be welcomed. That is precisely why he describes the debate on loosening as important and right, and he considers it very useful to set guidelines for distance, hygiene and masks. Durner emphasizes:
Meanwhile, his area has been able to analyse how the virus damages the lungs, Richter says: “In simple terms, one can say that the patient age is ‘no matter’ when it arrives in the lungs.” His clinic had determined early on that young people could also die from the virus. Based on data from the infected, an interdisciplinary team is now looking at the possible long-term consequences of different age groups.
Research in children’s boots
While politics and society talk primarily about easing and measures, research on coronavirus is still in the children’s boots. “At the moment, we only know what became known from the SARS pandemic 15 years ago. These include permanent, serious lung damage, “that was and is frightening,” Richter said. That is why good science is just as important as graduated and cautious relaxation of contact restrictions.
In order to be able to assess the situation professionally, studies are needed. “In principle, prevalence studies are an extremely important building block in pandemic assessment and are fundamental to many decisions,” Richter says. Despite the criticism of the Heinsberg study, this allows him to draw a conclusion if the re-assumed of just under 0.4 percent persists; death rate among those infected.
Based on the theory of herd immunity with 50 million infected people in Germany, about 200,000 deaths could be expected, “but they may spend 3 weeks in intensive care before that,” Richter notes. However, this is not the only reason why Richter does not seem practical:
But just as important as the diversity of reporting is that scientists explained their findings as understandably as possible. “No scientist can expect media representatives or the ‘ordinary citizen’ to understand scientific gibberish,” Richter says.
Communication must take place
The social and economic psychologist Prof. Dr. Anja Achtziger from the Zeppelin University in Friedrichshafen sees it in a similar way: “Large parts of science are financed by taxpayers’ money. Then the population should also see what is being done with it and how society benefits from it.” Especially in times and on topics in which people fall for unsubstantiated conspiracy theories, qualitative reporting is important at the same time – combined with an objective and objective argumentation of science. In complex contexts, this is not always easy. “But such communication must take place, especially in far-reaching crises.” Unresolved issues and several explanations for a phenomenon should also be addressed openly; For this, the population must also show patience and understanding: “Some things simply take time.”